Scientists have created a new kind of artificial cornea, inserting a sliver of collagen into the eye that coaxes its own natural corneal cells to regrow and restore vision.
It worked in a first-stage study of 10 patients in Sweden, researchers reported Wednesday. And while larger studies are needed, it’s a step toward developing an alternative to standard cornea transplants that aren’t available in much of the world because of a shortage of donated corneas.
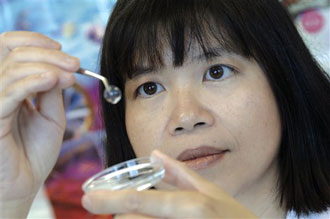
“We’re trying to regenerate the cornea from within,” said Dr. May Griffith, senior scientist at the Ottawa Hospital Research Institute in Canada and a professor of regenerative medicine at Linkoping University in Sweden.
Vision depends on a healthy cornea, the film-like covering of the eye’s surface that helps it focus light. Corneas are fragile, easily harmed by injury or infection, and about 42,000 people in the U.S. receive transplanted corneas every year. While that’s considered an adequate supply in this country, donated corneas aren’t available in many countries for the estimated 10 million people worldwide with corneal blindness. Transplants also bring risk of rejection.
In addition, researchers are working to improve plastic-like artificial corneas and to create stem-cell treatments that could spur corneal growth.
The new work, published in the journal Science Translational Medicine, is a bioartificial cornea — an attempt to use the same natural substances that make up a real cornea to induce healing.
“I characterize this work as a major advance in the direction that we need to go,” said Dr. Alan Carlson, cornea transplant chief at Duke University’s eye center, who wasn’t involved in the research. To “make this mimic donor tissue to the extent that your own cells ultimately become incorporated in this tissue, I think that’s the most exciting aspect.”
A cornea’s structure is made up of a tissue called collagen. First, researchers took human collagen grown in yeast, made by San Francisco-based FibroGen Inc., and molded it into a contact lens-looking shape — the scaffolding, essentially, for a cornea.
Then Griffith, working with Linkoping University eye surgeon Dr. Per Fagerholm, studied the bioartificial cornea in 10 patients with severe vision loss from damage to a corneal layer. Damaged tissue in one eye was removed, and the new biosynthetic cornea implanted. Soon, cells that line a healthy cornea started growing in the collagen. Tear production normalized, and even corneal nerves regrew, something researchers could test by measuring sensitivity. There was no rejection, and patients didn’t need immune-suppressing medication.
Two years later, six of the patients had significantly improved vision with glasses and two were no worse. When implanted with contact lenses that previously they couldn’t tolerate, patients saw as well as a similar group of patients who had received standard corneal transplants.
Duke’s Carlson cautioned that these weren’t full-thickness corneal transplants — the lowest layer of the patients’ original corneas wasn’t replaced. People with these more upper-layer corneal problems make up about 10 percent of transplant cases, he said, while the bigger hurdle is creating therapy for harder-to-treat full-thickness damage to what’s called endothelial cells.
But he called the experimental technology a step toward that goal, and Griffith said she is planning larger studies and will try to extend the therapy to a wider range of vision loss.